Ocularist
This probably a profession you have never heard of, but if you are smart enough you have already noticed it’s a speciality because it ends with the suffix -ist. Actually, when I first saw it, I knew it was something fascinating. So you are not alone
This probably a profession you have never heard of, but if you are smart enough you have already noticed it’s a speciality because it ends with the suffix -ist. Actually, when I first saw it, I knew it was something fascinating. So you are not alone.
What does an Ocularist do?
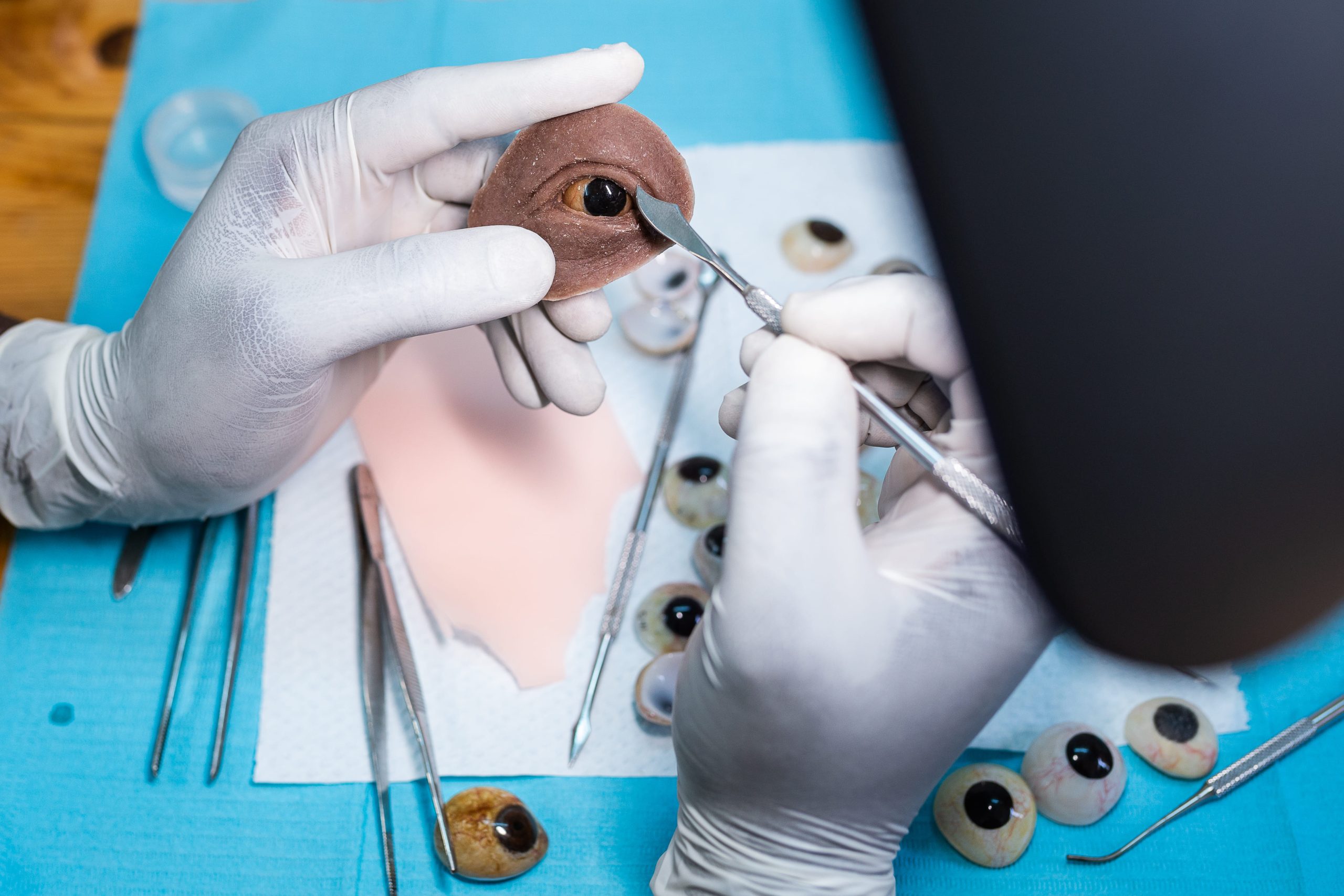
An Ocularist is a thoroughly trained professional skilled in the art of fitting, painting and fabricating custom ocular prostheses. In addition to creating custom ocular prostheses, and providing long-term care through periodic examinations, an ocularist provides the patient with complete instructions on the care and maintenance of their prosthesis.
They are considered an artist because they shape and paint the prosthesis to appear lifelike and to ideally be unnoticeable when observed.

What’s the difference between “stock” and “custom” artificial eyes?
“Stock” or “ready-made” ocular prostheses are mass-produced. Since a “stock eye” is not made for any particular person, it does not fit or match in colour. A “custom” ocular prosthesis, on the other hand, is specifically made by an Ocularist to fit and match a patient’s companion eye in all aspects. A custom artificial eye is also designed to promote the long-term health and development of the patient’s socket. A “stock-eye” does not.
Patients who need to be referred to an Ocularist usually fall into the following categories,

| M | T | W | T | F | S | S |
|---|---|---|---|---|---|---|
| 1 | ||||||
| 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| 9 | 10 | 11 | 12 | 13 | 14 | 15 |
| 16 | 17 | 18 | 19 | 20 | 21 | 22 |
| 23 | 24 | 25 | 26 | 27 | 28 | |
Search
Recent enucleation/evisceration (eye removal).
Post Operative Patients normally, patients who have had an enucleation or evisceration should be referred to the Ocularist for the fitting of the ocular prosthesis 6 to 8 weeks postoperatively. This period allows for sufficient healing and a stable socket. Although patients healing rates vary by the technique and implant material used, age, previous treatments and other medical conditions, the anophthalmic socket or eviscerated globe is ready for fitting when chemosis and orbital inflammation have fully resolved. The impression fitting will be invalid if a significant change in the orbit occurs after the impression is taken. As an interim measure, the patient can be referred at around 4 weeks following surgery for evaluation of the fit of the postoperative conformer, to either fit a better fitting conformer, or fit a temporary prosthetic eye. This also allows the patient to be introduced to the Ocularist and the fitting and fabrication procedures.
Problems with an existing prosthesis.

Patients with existing ocular prostheses will often need to be referred to the Ocularist for problems with either the surface condition of the prosthesis or problems with the fit of the prosthetic eye or scleral shell.
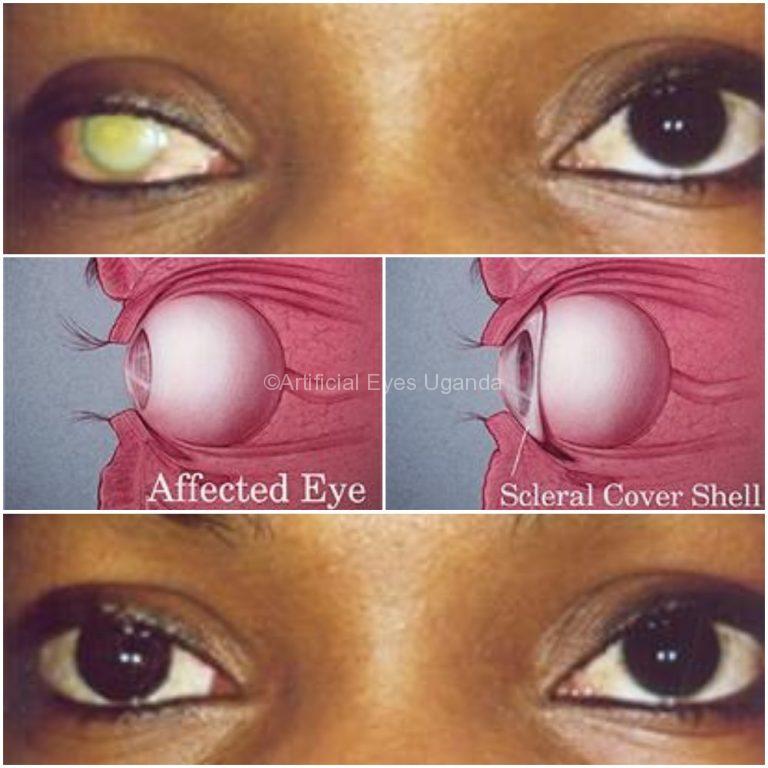
Blind eyes requiring a scleral shell.
Surface Condition Problems
With continuous wear of an ocular prosthesis, there is a build-up of a protein film on the surface of the prosthesis. This is normally cleaned off by the patient during a 1-to-3 month interval. This time span varies with each individual and can even vary throughout the year for the individual patient. With overextended wear, the protein build up can be quite encrusted and difficult to clean. The Ocularist often needs to polish off the stubborn surface deposits.
With normal wear and handling of the ocular prosthesis, it is not uncommon to acquire fine, hairline scratches in the plastic surface of the prosthesis. The scratches and other surface defects can be caused by many factors and need to be professionally polished out by the Ocularist.
Poor Fit Of The Ocular Prosthesis/Sceral Shell
The fit of a prosthetic eye or scleral shell will deteriorate over time. The average life of an ocular prosthesis is 5 years. The most common reasons for prosthetic eye replacement is a poor fit due to orbital fat atrophy and implant migration resulting in a recession of the prosthesis with the corresponding narrowing of the palpebral fissure. In addition, the comfort of the prosthesis is often affected. With a scleral shell, continued phthisis or other changes in the globe may be contributing factors.
Children will often need more frequent replacements and/or enlargements to compensate for growth and help stimulate bony orbital growth.
Conditions of socket contracture, lagophthalmos, ptosis, lower lid laxity, entropion, ectropion, implant exposure, and other conditions can often be improved or minimized with the appropriate prosthetic modifications. In some cases, enlargement or reduction of the prosthesis is indicated and in other cases, replacement is the appropriate choice.
Blind Eyes Requiring Scleral Shells
Scleral cover shells are fitted over the conditions of phthisis bulbi, evisceration, congenital microphthalmia, and the normal sized, blind, disfigured eye. Scleral shells differ from prosthetic eyes in their thickness and length of wearing time depending on the size and sensitivity of the eye. If there are questions of successful wear of the scleral shell due to corneal sensitivity, they can be answered with a consultation with the Ocularist and may involve the fitting of a clear trial shell.
Congenital anophthalmia/microphthalmia.
In cases of congenital microphthalmia and more importantly, congenital anophthalmia, it is important to refer the infant/child to the Ocularist as early as possible to start the fitting of conformers and/or prostheses to help stimulate bony orbital growth. Fitting of a series of increasing larger prostheses will help to minimize the hypoplasia and form an adequate socket. Normally, the only limiting factor is the stenotic palpebral fissure, but with time and non-surgical prosthetic augmentation, a good result is achieved. EUAs for impressions and/or fittings of larger shapes may be needed

Services Provided By The Ocularist.
The following summary will be of help in assessing the appropriate service to be requested by the ophthalmologist of the Ocularist.
- CLEANING: as needed (1-3 month average) normally done by the patient
- POLISHING: 1-2 times a year depending on patient care
- ENLARGEMENT: within first 1-3 years of the life of prosthesis or due to growth
- REDUCTION: as indicated due to socket contracture, lagophthalmos, etc.
- REPLACEMENT: 5 years or as needed when a change in fit, comfort, cosmesis

ABOUT US
We take great passion in creating solutions that can give you so much confidence and encouragement in a situation that can at times be very difficult. We are all highly motivated professionals, constantly working to produce prostheses, the best each time we do it. We remain well connected with those in our industry, to evolve in the best we can be while learning from others.
FOLLOW US
ALL CONTACTS
- Queen's Road, Entebbe
- +256754077479
- contact@artificialeyesuganda.com
- Only On Appointment
- P.O.Box 738, Entebbe, Wakiso, Uganda
- Artificial Eyes - Copyright 2021












Leave a Reply